A new study from researchers at Stanford University School of Medicine reports that gastrectomy surgery, a type of weight loss operation, has an impact on testosterone levels in obese men. The results, demonstrating that the procedure normalizes testosterone levels over a 12-month period, were presented at the 2015 Clinical Congress of the American College of Surgeons. The study, entitled “Benefits of bariatric surgery do not reach obese men” was published in the Journal of the American College of Surgeons.
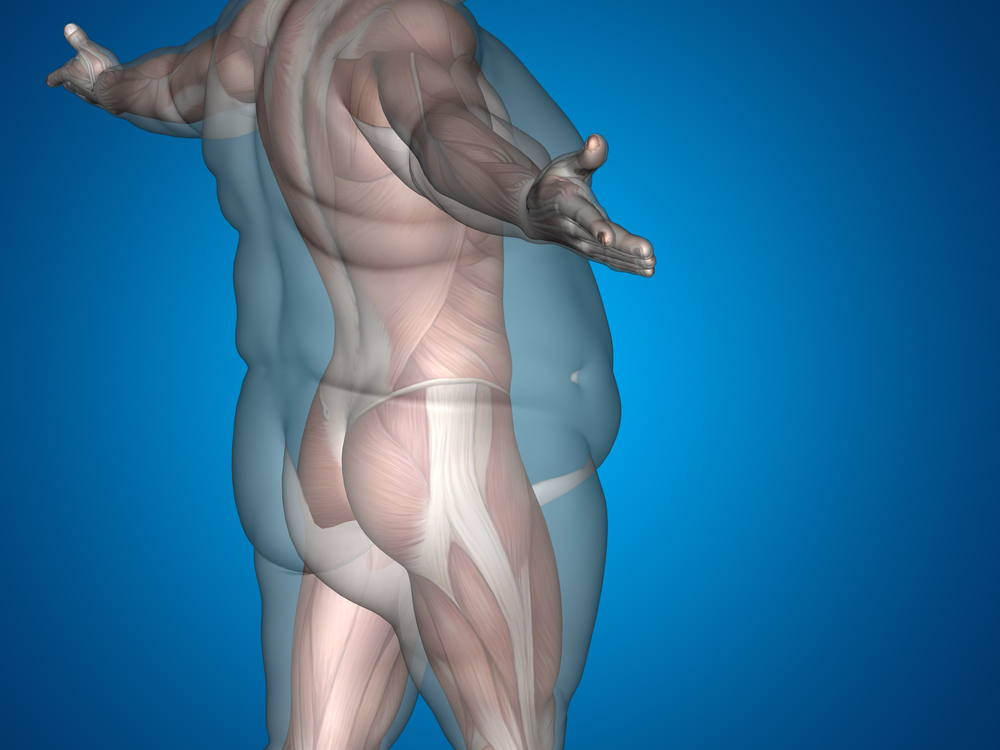
Obese men have low levels of testosterone due to the conversion of fat to estrogen that drives testosterone levels down. Besides the obvious negative impact on the patient’s sex life, low testosterone is also a risk factor for cardiac disease, sarcopenia (loss of muscle tissue, leading to a more rapid aging process), an increased propensity for weight gain, and poor quality of life.
Researchers investigated the effect of sleeve gastrectomy on levels of the precursor of testosterone (DHEA), serum testosterone and prostate-specific antigen (PSA) in 24 obese male patients at months 3, 6 and 12. This surgical procedure consists of the removal of about 75% of the stomach, leading patients feeling satisfied with less amount of food, and is also safer and offers faster results than gastric bypass.
Primary results indicate that after the procedure the subjects experienced an increase in serum testosterone levels, on average going from 295 to 423 ng/dL at 12 months, a value that reaches the normal range of circulating testosterone, 300 to 1000 ng/dL. Only 41% of patients presented with low testosterone, as opposed to 63% before the procedure. DHEA and PSA concentrations also rose from 12.8 to 39.6 ng/mL and 0.62 to 0.75 ng/mL, respectively. Importantly, no change in PSA mass was observed, an important biomarker for prostate cancer. Body mass index (BMI) was also decreased from 46 before surgery to 31 after surgery.
RELATED : ORBERA Intragastric Balloon Non-Surgical Weight Loss Device Receives FDA Approval
Co-author John Morton, MD highlighted the importance of this study, especially regarding male benefit in undergoing such surgery, “The take home message is that if you are an obese man with low testosterone your therapy should be weight loss not testosterone replacement, and a successful way to achieve meaningful weight loss is through a bariatric operation,” Dr. Morton explained “This is a unique and beneficial finding for sleeve gastrectomy hasn’t been studied before, demonstrating for the first time, that testosterone levels are improved in a group of obese male patients following sleeve gastrectomy.” Currently, only about 20% of obese patients that undergo weight-loss surgery are men, although obesity rates are similar between gender.