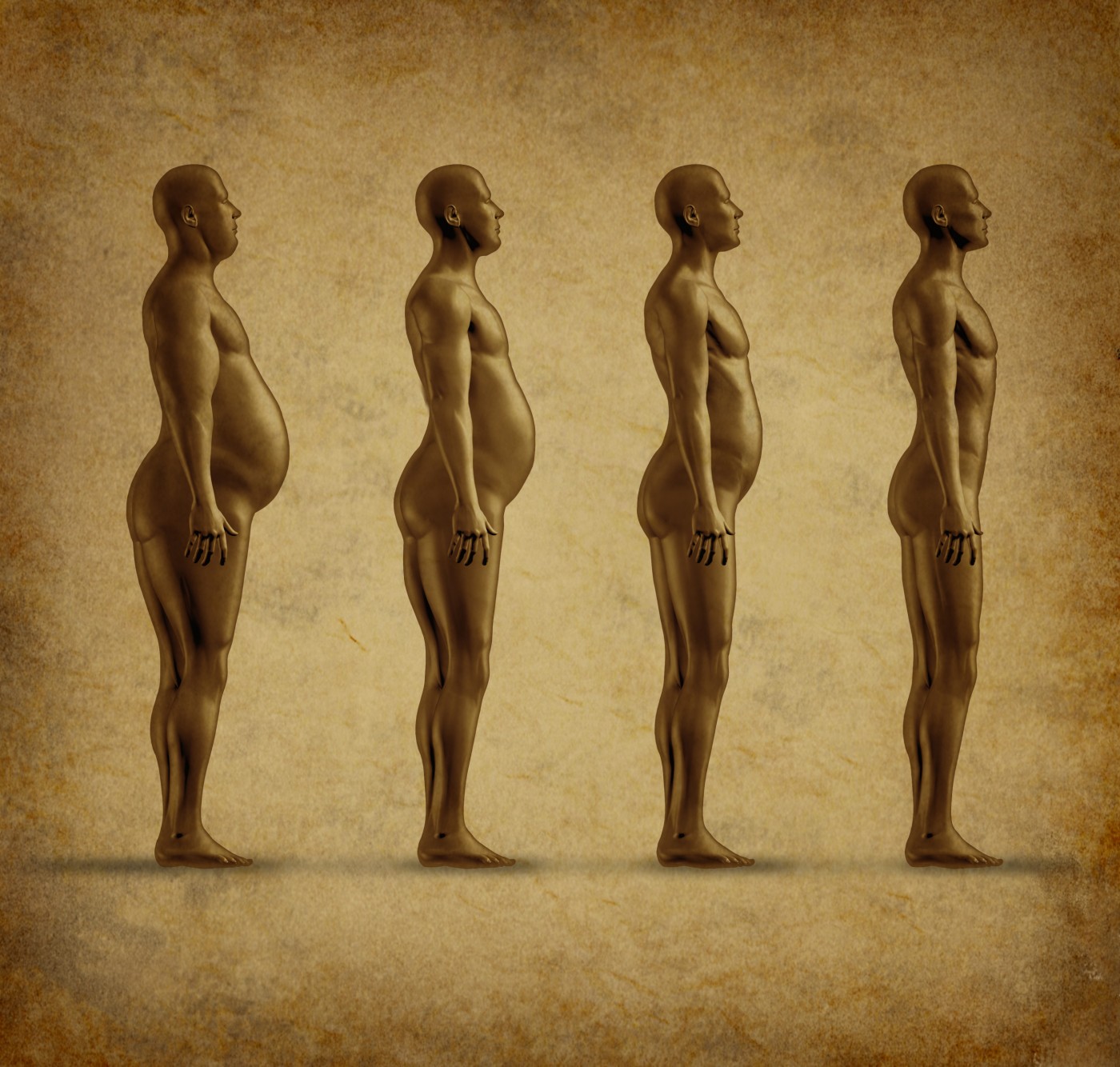
Five-year results from a multicenter clinical trial investigating the safety and efficacy of LAP-BAND® adjustable gastric banding system in patients with a body mass index (BMI) of 30–39.9 kilograms per square meter are complete, and show that patients experienced significant weight loss and beneficial health outcomes. These data support the one-year trial that allowed the patients indicated for LAP-BAND to expand from only those with a BMI of at least 40 kilograms per square meter, or a BMI of at least 35 kilograms per square meter with a severe comorbidity, to also include patients with a BMI of at least 30 kilograms per square meter.
“Obesity has become a critical health issue in the United States and this study shows the LAP-BAND® System is a viable, safe alternative for patients who have been unsuccessful at weight loss and want to improve their quality of life,” said John Morton, MD, Director of Bariatric Surgery at Stanford University Hospital and Clinics, in a news release provided to Obesity News Today by Apollo Endosurgery, Inc. “For many, the weight loss journey leaves patients with little support or options. Gastric banding can be successfully implemented before patients become severely obese and can enable positive, lifelong outcomes.”
As described in “LAP-BAND® for BMI 30-40: 5-year Health Outcomes from the Multicenter Pivotal Study,” which was published in International Journal of Obesity, 149 patients received a LAP-BAND and were followed for a span of five years. Each patient was assessed after surgery for effectiveness and adverse outcomes at follow-up appointments, which took place after one week; during months one, two, four, six, 10, 12, 15, 18, 21, 24; and every six months following the two-year mark. Effectiveness was defined as a loss of at least 30% of excess weight in at least 40% of the study population.
“This paper showcases the clinical efficacy of the LAP-BAND® System for long-term weight loss and reinforces Apollo’s commitment to providing obese patients with proven weight loss options through minimally invasive medical procedures,” said Dennis McWilliams, President and Chief Commercial Officer of Apollo Endosurgery.
The LAP-BAND appeared to be more than adequately effective, as 76% of patients experienced an excess weight loss (EWL) of more than 30% of their excessive weight. This changed the rate of obesity in the study’s patient population from 99.3% to 36.2% at the final mark. The five-year rate was slightly higher than the two-year rate identified previously, which was 34.3%. The study showed mean percent weight loss at five years was 15.9 +/-12.4%, corresponding with 62.7% EWL during the study period. Previously released data from the study showed 65% and 70% EWL after one and two years, respectively. Secondary endpoints were also measured and showed benefits in comorbidities that included 85.7% improvement in diabetes, 64.4% in dyslipidemia, and 59.6% with hypertension.
Researchers believe that the LAP-BAND is effective in treating obesity because it leads to greater satiation and fullness during meals, helping to prevent patients from binge eating. The weight loss device may also help patients make better decisions about food, since according to the results of functional magnetic resonance imaging (fMRI) of the brain, LAP-BAND patients encountering visual food cues have reported higher-level perception in their brains. With these suggested mechanisms and efficacy data in hand, the researchers believe that it is important to intervene early in obesity onset, and that the LAP-BAND can be an appropriate option for patients with a BMI of 30–39.9 kilograms per square meter.