According to a study published in the Journal of the Academy of Nutrition and Dietetics, depression increases the risk of poor nutrition and obesity among Americans receiving food assistance.
According to a study published in the Journal of the Academy of Nutrition and Dietetics, depression increases the risk of poor nutrition and obesity among Americans receiving food assistance.
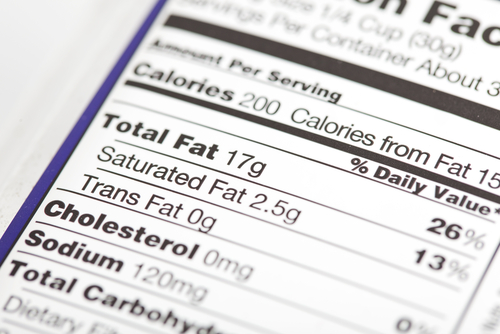
In their study entitled “Associations between Depressive Symptomatology, Diet, and Body Mass Index among Participants in the Supplemental Nutrition Assistance Program,” Karen Florez and colleagues examined the relationship between depressive symptomatology, dietary quality, and body weight among a sample of Supplemental Nutrition Assistance Program (n=639). Data was collected from May to December 2011 by trained data collectors. The participants’ main food shop preferences were in low-income “food deserts” in Pittsburgh. Food deserts refer to neighborhoods with limited access to healthy foods, such as fresh produce.
Results revealed that depression is a strong and statistically significant predictor of both dietary quality and BMI; higher score in depressive symptomatology was associated with lower scores in dietary quality. A higher score in depressive symptomatology was associated with higher BMI.
These findings show that there is an association between depressive and weight-related outcomes and indicates that a comprehension of the risk of depression in SNAP participants could be relevant to understanding the relationship among SNAP participation, diet, and weight. However, the researchers did not find a causal relationship between depression and bad eating habits or obesity.
The association between depressive symptomology, elevated BMI, and lower dietary quality among low-income, primarily African-American residents living in a food desert suggests the need for mental health interventions to have broader benefits in this population. However, further research is needed to determine if eating a healthier diet and controlling weight may improve mental health in this group of people.
“This study focuses on a group that is of particular importance: low-income, primarily African-American residents of urban food deserts,” lead investigator Karen Florez, an associate social scientist at the Rand Corp., said in the news release.
“This group is at particularly high risk of obesity and poor nutrition,” she added. “Thus, the finding that depression is associated with even higher risk within this already high-risk group suggests a potential avenue for intervention is a focus on mental health.”