Findings from a recent study indicate that heart function in patients with morbid obesity returns to normal after bariatric surgery, but not after lifestyle interventions. The results suggest that bariatric surgery may decrease the risk of cardiovascular disease in these patients. The study, published in the European Journal of Preventive Cardiology, is titled, “Effect of weight loss on subclinical myocardial injury: A clinical trial comparing gastric bypass surgery and intensive lifestyle intervention.”
“Obesity is a global problem that is closely linked to the development of cardiovascular disease,” said lead author, Dr. Magnus N. Lyngbakken, a PhD candidate at the University of Oslo in Norway, according to a news release. “Morbidly obese patients are at high risk of heart attack, heart failure, and diabetes.”
Although diets and other lifestyle interventions may have beneficial cardiometabolic short-term effects, they have proven relatively ineffective in the long term, particularly in morbidly obese patients.
Cardiac troponins are commonly used to diagnose acute ischaemic injury, as well as to determine if a patient had a heart attack. Recent advances in cardiac troponin assay methodology permit measurement of detectable circulating levels in large proportions of the general population.
Several studies have also reported an association between troponin concentrations and body mass index (BMI). Moreover, high-sensitivity troponin I (hs-TnI) and T (hs-TnT) have both been shown to be strongly associated with the risk of heart failure and cardiovascular death in patients with stable coronary artery disease, as well as in the general population.
Researchers examined the effect of weight loss induced by bariatric surgery and by intensive lifestyle interventions on levels of circulating high-sensitivity cardiac troponin I in patients with morbid obesity, which would indicate cardiac stress and chronic subclinical cardiac injury.
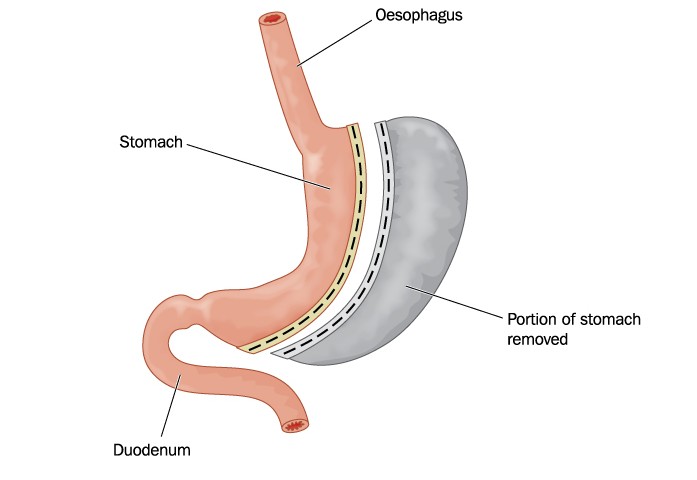
The researchers measured hs-TnI concentrations pre- and 12 months post-intervention in 136 subjects with morbid obesity participating in a controlled clinical trial comparing the effect of intensive lifestyle intervention (n=62) with Roux-en-Y gastric bypass (n=74). The researchers also included a control group of people with normal weight (n=30).
At baseline, median high-sensitivity cardiac troponin I levels were 2.40 ng/L in the bariatric surgery group, 2.35 ng/L in the intensive lifestyle intervention group, and 0.90 ng/L in the normal weight group.
At 12 months after the intervention, hs-TnI levels decreased significantly in the surgery group but not in the lifestyle group.
On average, the surgery group lost 30% of their body weight while the lifestyle intervention group lost 8%. “The extensive weight loss that we saw with the surgery group was associated with a drastic reduction in hs-TnI levels,” said Dr. Lyngbakken. “The group that exercised and ate less showed no such significant reduction in levels of hs-TnI.”
After 12 months, the hs-TnI levels in the bariatric surgery group were also not significantly different from the normal weight group. However, in the intensive lifestyle intervention group, hs-TnI levels remained significantly higher compared with the control group.
“Twelve months after surgery levels of hs-TnI were the same in the surgery group as in the control group of normal weight,” said Dr. Lyngbakken. “It’s too early to tell, but if this translates into less heart failure, heart attacks and cardiovascular deaths, then this could mean that morbidly obese patients who have bariatric surgery obtain a cardiovascular risk comparable to a normal weight population.”
“This is one of the first studies showing that an intervention can reduce mildly elevated cardiac troponin levels,” said author Professor Torbjørn Omland, professor of medicine at Oslo University. “High-sensitivity troponin I is a good marker of how much stress the heart is exposed to. Marked weight loss induced by bariatric surgery seems to have a direct effect on the health of the heart and reduces strain to normal levels.”
Results from multivariate analysis further revealed that surgery was a predictor of high-sensitivity cardiac troponin I level reduction even after the researchers adjusted for age, gender, and other variables. Subsequent multivariate analyses showed that reductions in body weight and triglycerides were potential mediators of reduction in hs-TnI circulating levels.
“Bariatric surgery reduces the stress on the heart through a reduction in body weight. It also improves the cardiometabolic milieu of the body, as reflected by the drop in triglycerides, which has beneficial effects on heart muscle cells,” Professor Omland said. “Our findings and those of other studies all point to bariatric surgery being superior to lifestyle intervention with regard to the beneficial effects on the heart. Much of that can be explained by the greater weight loss induced by bariatric surgery. Although lifestyle intervention leads to a transient reduction in weight, its impact in the long term is not as great as surgery.”